Department of Midwifery

Dr. Tiran Jamil Piro
Lecturer
Head of Midwifery Department
Introduction
Midwifery Department which established in 2012 after applying for DelPHE Iraq, round two 2010 project, which is supported by British Council to establish a midwifery program at Hawler Medical University, College of Nursing. Faculty of Health and Medical Sciences, Division of Health and Social care, University of Surrey, UK, helped the college to prepare a BSc midwifery curriculum. The curriculum was approved. This department still is unique academic unit which provide BSc in Midwifery to it’s students in Kurdistan and Iraq. The Bsc Midwifery is a full-time four year program, offered by the department of Midwifery, college of Nursing, Hawler Medical University. Clinical placements take place in the Maternity Teaching Hospital and primary Health care Centers in Erbil City, Kurdistan Region, Iraq. Certified midwives manage women's health care focusing on pregnancy, childbirth postpartum, care of the newborn and family planning and gynecological needs of women as well as specialty care and support for expecting mothers. Upon graduation, midwives practice in a variety of settings including primary health care centers governmental hospitals, private hospitals and home birth services.
BSc, Midwifery
The Bsc Midwifery is a full-time four year programme, offered by the department of Midwifery, college of Nursing, Hawler Medical University. Clinical placements will take place in the Maternity Teaching Hospital and primary Health care Centers in Erbil City, Kurdistan Region, Iraq. Certified midwives manage women's health care focusing on pregnancy, childbirth postpartum, care of the newborn and family planning and gynecological needs of women as well as specialty care and support for expecting mothers. Upon graduation, midwives practice in a variety of settings including primary health care centers governmental hospitals, private hospitals and home birth services.
Philosophy
Midwives believe that health is a human right and that an investment in maternal and child health safeguards the wellbeing of women, their families and the communities. The process of human childbirth is a normal physiological process. Women should have as much control as possible in determining their care, and should be encouraged to be active participants in decision-making and self care. Midwifery is both an art and a science. The art of midwifery consists of sensitivity to the needs of women and families and being able to meet these needs in the most appropriate way. The science of midwifery overlaps with that of other disciplines such as nursing and medicine. We see our clients as whole, capable people for whom the processes of pregnancy, labor delivery and parenting offer the opportunity for significant personal growth.
Vision statement
The midwifery programme will produce midwives able to provide comprehensive quality maternal and child health services continued competency for practice requires that each midwife commits herself to an on-going process of life-long education.
Mission statement
Midwifery program in the college of nursing, Hawler Medical university is to prepare midwives at an advanced level in essential competencies for basic midwifery practice. Knowledge, attitudes, skills and practices at all levels of the health care system according to professional standards.
Programme goal
The bachelor of science in midwifery education programme aims at preparing the student to be competent midwives who will play a vital role in improving the quality of life of childbearing families. The teaching and learning process facilitate student's skill development, decision-making capacity and application of competencies based on service and profession led education.
Programme objectives
On successful completion of this programme, the student will have acquired the knowledge, attitude, skills and practices which will enable them to:
1. Collect information to critically analyze social determinants and epidemiological patterns for improving maternal and newborn health outcomes.
2. Utilize appropriate counseling and communication skills to interact effectively with women, children and their families.
3. Integrate the concepts of midwifery process in planning and providing care for women during pregnancy, intrapartum, postpartum and for the newborns.
4. Uphold midwifery care and its relevance in the care and management for childbearing women and their families.
5. Apply reflective models to drawn lessons from personal experience about own clinical practice in emergency obstetric and neonatal care for mothers and babies.
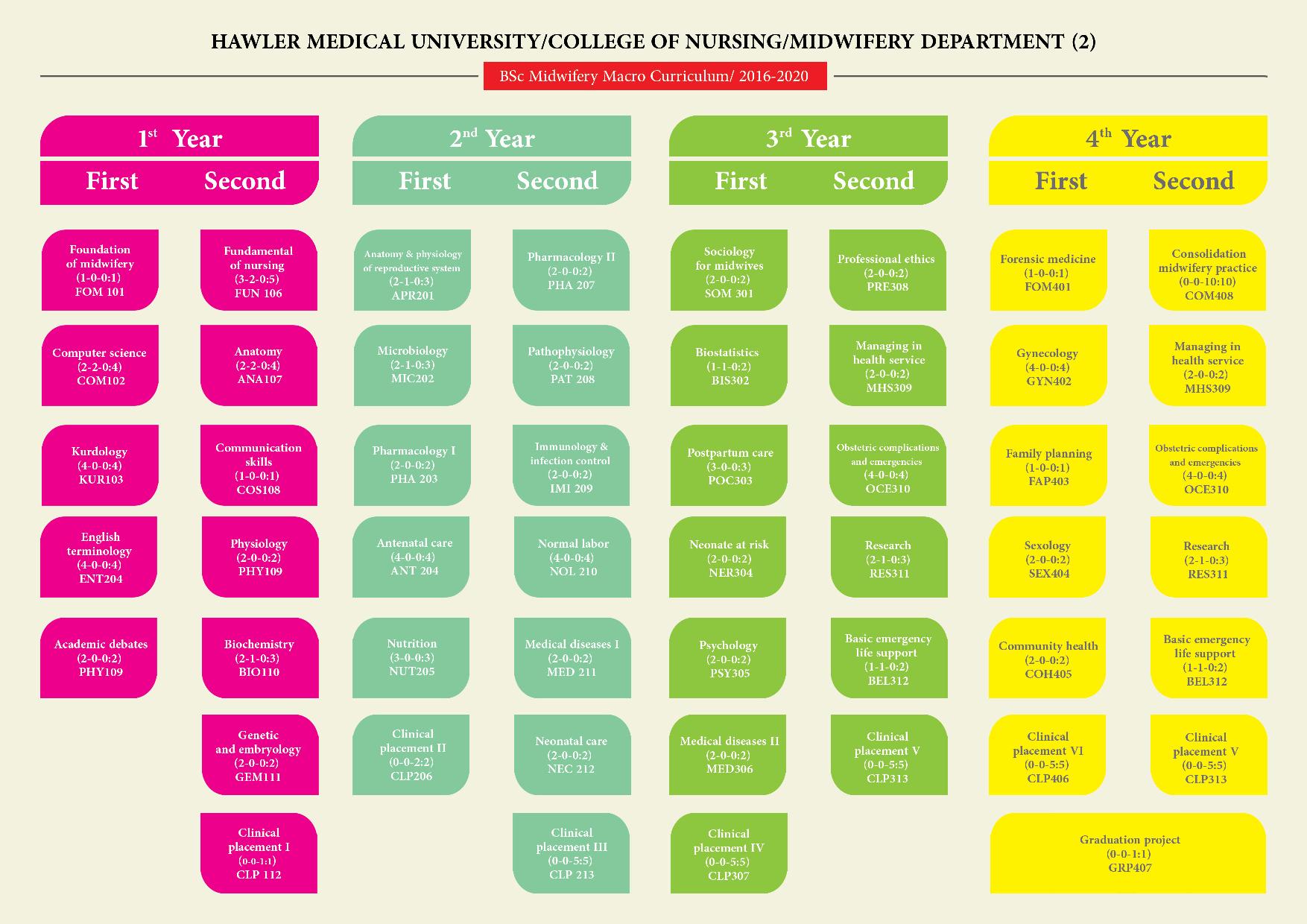
Midwifery Curriculum
Graduation requirements
Graduates must meet the following minimum clinically requirements:
Essential requirements for graduation of BSc students of midwifery
|
|
Requirements |
Total number |
Details |
Subtotal number |
Form No. |
|
1
|
Antenatal care |
100 |
Provide antenatal care to normal mothers |
70 |
F.1 |
|
Provide antenatal care to high risk mothers |
30 |
F.1 |
|||
|
2 |
Performing vaginal delivery |
40
|
Conduct normal vaginal deliveries of primiparus women |
20 |
F.2 |
|
Conduct normal vaginal deliveries of multiparus women |
20 |
F.2 |
|||
|
3 |
Performing abnormal vaginal deliveries |
5 |
Breach, placenta previa, preterm labor, stillbirth,... |
5 |
F.2 |
|
4 |
Performing and suturing episiotomy |
20 |
Suturing episiotomy |
20 |
F.3 |
|
5 |
Post partum care |
50 |
Provide postpartum care to normal mothers - Maternity hospital - Health center |
25 10 |
F.4 |
|
Provide postpartum care to high risk mothers |
15 |
F.4 |
|||
|
6
|
Neonatal care |
50 |
Perform neonatal examination (postpartum unit) |
40 |
F.5 |
|
Assist in neonatal resuscitation |
10 |
F.6 |
|||
|
|
|
|
Gynecological exam |
30 |
F.7 |
|
7 |
Gynecological examination |
50 |
Clinical Breast examination |
10 |
F.8 |
|
Take pap smear |
10 |
F.9 |
|||
|
8 |
Family planning |
20 |
Contraceptive consultant |
15 |
F.10 |
|
Assist in IUD insertion
|
5 |
F.11 |
Comment: Medication chart (Form no. 12) are filled with all other forms. Parthograph (Form no. 13) are filled with vaginal delivery forms. EPDS (Form no. 14) are filled with postpartum forms in health center.
College of Nursing
Midwifery Department
This is to certify that
……………………………………………………………..
has completed all following essential clinical requirements for graduation in BSc Midwifery in the Academic Year 2016-2017.
- Provide antenatal care to normal and high risk mothers ………………………………………70 cases
- Conduct normal vaginal deliveries of primiparus and multiparous women …………. 40 cases
- Conduct abnormal vaginal deliveries………………………………………………………………….……5 cases
- Performing and suturing episiotomy ……………………………………………………………………..20 cases
- Provide postpartum care to normal and high risk mothers ……………………………………50 cases
- Perform neonatal examination ……………………………………………………………………………..40 cases
- Assist in neonatal resuscitation……………………………………………………………………………..10 cases
- Perform gynecology history and exam ………………………………………………………………….30 cases
- Perform breast examiniation ………………………………………………………………………………..10 cases
- Take pap smear …………………………………………………………………………………………………….10 cases
- Give contraceptive consultion ………………………………………………………………………………15 cases
Graduation requirements
The student will be competent to:
- Take full history of pregnancy and labor including the review of maternal pregnancy records.
- Perform a general physical examination to assess the woman's condition.
- Perform an abdominal examination to confirm the period of gestation, identify the lie, presentation, position and descent of fetus and auscultate the fetal heart.
- Assess the frequency, duration and strength of uterine contractions.
- Perform a vaginal examination to determine cervical effacement and dilatation, confirm whether or not the membranes have ruptured, identify the presenting part and position of the fetus, the moulding, the station and level of the head and rule out cephalo-pelvic disproportion.
- Accurately record the progress of labor and monitor maternal and fetal condition regularly throughout labor using the partogram.
- Interpret partogram records correctly, develop a comprehensive plan of care and critically evaluate the effectiveness of care given and take timely, appropriate action when there is any deviation from normal.
- Provide emotional support for the woman and her family, keep woman fully informed of progress and involving her in all decisions related to her care.
- Keep the woman in optimum condition during labor, maintaining adequate hydration and nutrition, ensuring that the bladder is emptied regularly, promoting high standards of infection prevention and appreciate the importance of pain relief.
- Recognize the signs and symptoms of the second stage of labor and provide constant care, observation and support, allowing non-directive pushing, providing support of the perineum and avoid interference with the normal mechanism of labor.
- Make and suture an episiotomy when indicated, apply a local anesthesia to the perineum prior to repair.
- Provide immediate care for the newborn, including drying, clearing airways, ensuring that breathing is established, and skin-to-skin contact with mother and covering to provide warmth.
- Contact correctly management of the third stage of labor including the active management of the third stage of labor, using oxytocin.
- After delivery of the placenta and membranes, ensure that the uterus is well contracted by rubbing up a contraction and expelling clots, if necessary, and checking that vaginal bleeding is minimal.
- Examin the vulva, perineum and lower vagina for lacerations, repair second-degree tears to specialized care.
- Estimate and record all blood loss correctly.
- Examine the placenta and membranes for completeness and normality and dispose of them safely as appropriate.
- Monitor the mother's condition, ensuring that vital signs and vaginal bleeding are within normal limits and that the uterus remains well contracted and retracted.
- Record all details of all the stages of labor.
- Assess for uterine involution and healing of lacerations/repairs.
- Initiate and support uninterrupted (exclusive) breastfeeding.
- Educate mother on care of self and infant after delivery including rest and nutrition.
- Identify hematoma and refer for care as appropriate.
- Counsel woman/family on family planning post delivery.
- Refer for selected complications.
- Develop a discharge plan in partnership with the woman and her family for follow-up postpartum.
- Record findings including what was done and what needs follow-up.
- Correctly perform an immediate assessment of the neonate at birth.
- Perform correct and timely resuscitation for an asphyxiated neonate at birth.
- Correctly perform a screening examination looking for signs of immediate neonatal problems.
- Begin emergency care and management for respiratory distress, hypothermia and hypoglycemia.
- Safely transfer the neonate to emergency care facility when available.
- Records findings, including what was done and what needs follow up.
- Support parents during transport/transfer of neonate.
- Assist the mother with counseling, attachment and positioning for successful breastfeed the infant.
- Educate parents about infant normal growth and development, daily care and management, prevention of infection and danger signs and when to bring the infant to the clinic for care.
- Develop a discharge plan together with the mother explaining on how to use it in practice.
- Initiate immunization programe as per local schedule.
- Assist parents to access community recourses available to the family.
- Support parents with multiple births.


